CONCARD
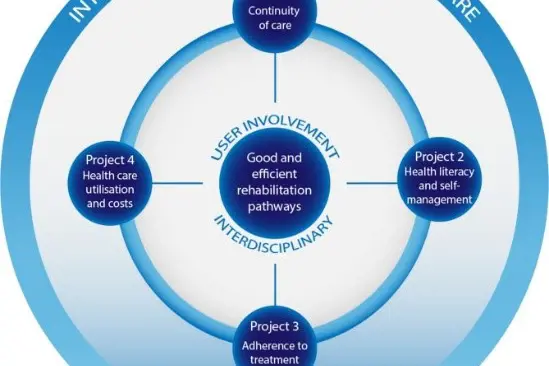
The overall aim of the CONCARDPCI study is to investigate continuity of care, patient preferences, adherence to treatment, cardiac rehabilitation participation and uptake, and health literacy and self-management in patients undergoing PCI. Further, to determine associations with future short- and long-term health outcome, health care utilization and costs. The study includes more than 3000 patients after PCI. Principal investigator of the study is professor Tone Merete Norekvål.

Annually, about 12 000 patients undergo PCI in Norway. Discharge from hospital to home is challenging for many patients. During this time, the patient has to consider and make decisions about relevant lifestyle changes and new medications. Several international studies have found that patients with cardiovascular diseases do not have satisfactory medication adherence regarding secondary prevention medications. In this study, there is a particular focus on this topic.
Health literacy involves the ability to gain access to, understand, and use health information, and is central to the CONCARDPCI study. Patient involvement in healthcare development is central to and especially important in today’s health policies. How electronic health (e-Health) solutions can be used to improve health literacy and medication adherence, is investigated.

Considering the size of this patient group, few of these patients participate in a cardiac rehabilitation program. The project provides a basis for alternative models of cardiac rehabilitation for large patient groups, including eHealth solutions. Close collaboration with end-users and healthcare professionals in both municipalities and the specialist healthcare services ensures transfer of knowledge to clinical practice. Through an interdisciplinary approach, the study will identify potential bottlenecks in the patient journey from a patient perspective, and lay the foundation for a more cohesive treatment course within acute treatment and further follow-up of these patients.
The project combines forces from primary healthcare services, patient organizations, Learning and Mastery networks and seven large university hospitals in Norway and Denmark.

Figure 1: H=PCI centres including the local hospitals in their catchment area.
Patients are followed up with self-reported data, 2, 6 and 12 months after PCI, and further with registry data for 10 years, or until death.
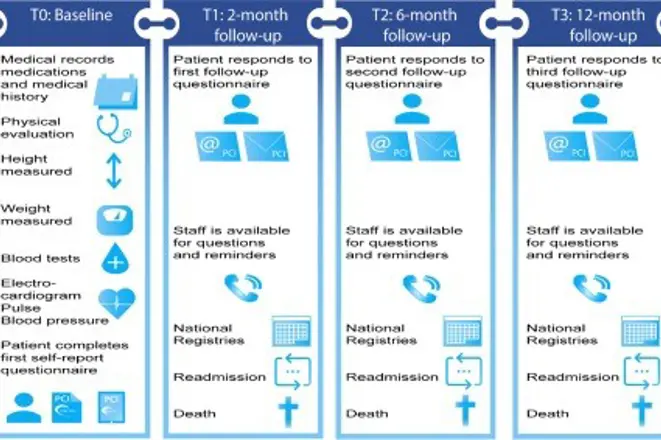
Figure 2: Measuring time points and data collection in the cohort study in CONCARDPCI.
The project is organized with a Research Team, Scientific Advisory Board (SAB), and an Expert Group with representatives from patient organizations and primary healthcare services. In addition, there are the teams of supervisors for the PhD-candidates.
| Scientific Advisory Board | Institution | Expertise |
| Heather Allore, PhD, Professor of Medicine (Geriatrics) and of Public Health (Biostatistics), and Director of the Yale Program on Aging Biostatistics Core | Yale University, USA | Design and analysis of studies of multi-component interventions and observational studies of multifactorial health conditions. |
| Christi Deaton, PhD, RN, FAHA, FESC, Florence Nightingale Foundation Professor of Clinical Nursing Research | University of Cambridge, UK | Wide clinical and research experience in acute cardiovascular patient care. Contributed to clinical practice guidelines development (European level). Participated in the COURAGE Trial. |
| Heather Hadjistavropoulos, PhD, Professor of Psychology | University of Regina, CA | Quality of healthcare across the continuum of care including integrated care pathways. Developed the HCCQ. |
Ann Dorthe Zwisler, MD, PhD, Professor of Medicine
| University of Odense, DK | Experience in programs of health and morbidity, rehabilitation and palliative programs. |
| Rikke Søgaard, MSc, MPH, PhD, Professor of Health economics | Aarhus University, DK | Econometric modelling for policy evaluation, and preference elicitation, and use of standardised measures for costs and outcomes measurement. |
Expert group
Through annual meetings in the Expert group, the project has established a broad collaboration with regional and local hospitals, rehabilitation centres, primary healthcare services, patient organizations, healthy Life centres, learning and mastery services, 24 municipalities and The Center for Health Research in Sogn og Fjordane. The main focus has been to develop an e-Health intervention to be used in cardiac rehabilitation.

Representatives from SAB, the Expert group, and the project group.
Prehospital symptom recognition and timely treatment of myocardial infarction
The purpose of the study was to explore patient’s experience of interaction with local hospitals and general practitioners, and their reflections on pre-hospital symptoms of myocardial infarction and how to act upon them, before admission to a PCI center. Twenty patients were interviewed prior to discharge from hospital.
The study shows that patients do not always take symptoms of acute myocardial infarction seriously, and that they misattributed and rationalized symptoms they were experiencing. They also delayed seeking medical assistance, and often chose to ignore chest pain. However, severe chest pain triggered an immediate need for care and patients acted immediately and called the emergency services.
Frequently, patients experienced a lack of timely treatment and delays in continuity of care in the patient journey. Regarding myocardial infarction, time is of the essence to achieve a good therapeutic result. Thus, healthcare personnel, both in primary and secondary healthcare services, must focus on rapid identification of symptoms of a myocardial infarction, and prevent delays in the critical care medicine pathway.

Medication adherence after PCI
The aim of the study was to explore patients’ experiences in adhering to a medication regimen after PCI and to explore which strategies or resources they employed if problems arose. In-depth interviews were conducted with 22 patients (12 men) aged 33-82 years of age, who had undergone PCI six to nine months earlier.
The reasons for medication non-adherence were multidimensional and interacting, and included intentional and unintentional reasons, side effects from medications, scepticism towards generic drugs, lack of information regarding seriousness of coronary artery disease after PCI, and the psychological impact of living with coronary artery disease. Furthermore, patients experienced that established routines and aids like a pill box were necessary to adhere to their medication regime. Findings from the study underline the need for a more structured follow-up care after discharge from hospital in order to improve medication adherence after PCI.

Patients’ experiences with the continuity of care in healthcare services after PCI
The aim of the study was to to explore how patients undergoing PCI experience continuity of care between secondary and primary care settings after early discharge. In-depth interviews of 22 patients (13 men) were conducted six to eight weeks after PCI.
Patients were satisfied with the technical treatment they received. However, the discharge process was described as fragmented, continuity of care across sectors was described as unstructured and unplanned, and there were patients who had not received any offers of cardiac rehabilitation or follow-up from their general practitioner. The study shows that there is a need for a more patient-centred follow-up care, interdisciplinary collaboration, and self-efficacy for patients who have undergone PCI.
eHealth solutions as a measure for improving cardiac rehabilitation programs
The aim of this systematic review article was to describe the effectiveness of e-Health solutions on secondary prevention of coronary artery diseases. Twenty-four intervention studies, with 3654 participating patients, were included.
Eight studies utilized m-Health technology to deliver secondary prevention programmes, nine studies utilized web-based technology, and seven studies utilized a combination of m-Health technology and web-based technology. Most of the studies utilized two or three components for their secondary prevention programme. Patient education was performed in twenty-one studies. m-Health technology were found to have a positive effect on medication adherence. Several studies including traditional cardiac rehabilitation programmes, showed improvement on heart-related risk factors.

The study found that evidence exists to support the use of e-Health secondary prevention programmes for patients with coronary artery disease, However, there is great variability in components and outcomes within the different modes of delivery. Therefore, larger studies are needed to determine the most efficient mode of delivery and components capable of addressing a favourable outcome for patients.
Read the article
Heart Continuity of Care Questionaire (HCCQ)
The Canadian questionnaire (HCCQ) that measures patients’ experiences with continuity of care and coherent health services, has been translated and validated into Norwegian. International translation procedures were followed, and user representatives and clinical experts participated in the work. The questionnaire has exhibited good psychometric properties (validity and reliability), but an confirmative factor analysis showed a moderate adaptation to the three continuity dimensions in the questionnaire (information, relation and leading continuity).
When evaluating construct validity, some interesting connections were found between continuity, participation in cardiac rehabilitation, and follow-up at the general practitioner’s. Systematic reviews emphasize the need for more research on the transition between healthcare services, and questionnaires like HCCQ can contribute to mapping the need for more integrated services for this patient group.
Modifiable risk factors and self-reported health after percutaneous coronary intervention: with and without a history of atrial fibrillation
The aims of this study were to determine and compare changes in modifiable risk factors and self-reported health in patients with and without a history of atrial fibrillation (AF) after percutaneous coronary intervention (PCI). This study is part of the CONCARDPCI, a prospective multi-centre cohort study including 3417 patients after PCI. Of these, 408 had a history of AF.
Patients with AF were older, more often male, and more often lived alone. In the follow-up period, the proportion of smokers increased in patients with a history of AF, however, decreased in patients without AF. Most of the patients with and without a history of AF did not adhere to the recommended minutes of physical activity per week. The patients with a history of AF reported poorer health at baseline. However, the physical and mental health improved over time in both groups after PCI. The patients with a history of AF reported more emotional reactions and insecurities.
An intensified focus on lifestyle interventions is needed to improve modifiable risk factors and self-reported health in patients with and without a history of AF after PCI.
Continuity and coherent health services after completed PCI
The aim of the study was to determine multifaceted aspects of continuity of care and their associations with socio-demographic characteristics, self-reported health, clinical characteristics and follow-up services for patients after PCI. In total, 1695 patients were included in the study, and 78% completed the Heart Continuity of Care Questionnaire two months after discharge from hospital. The patients reported that they were given too little information about lifestyle changes, medications and follow-up care in primary healthcare services after discharge from hospital.
Gender, written patient information, transfers to another hospital, follow-up at general practitioners and sufficient consultation time after discharge from hospital, were all significant factors regarding the patients’ experience of continuity of care. Women and patients who experienced more symptoms or problems after the cardiac event scored significantly worse on continuity. Patients experiencing acute clinical pathways scored better on continuity of care than patients experiencing planned clinical pathways. The study shows that there is a need for clearer structures and systems across service levels to ensure further follow-up care and rehabilitation.
Read the article
eHealth solutions as a measure for improving cardiac rehabilitation programs
The aim of this systematic review article was to describe the effectiveness of e-Health solutions on secondary prevention of coronary artery diseases. Twenty-four intervention studies, with 3654 participating patients, were included.
Eight studies utilized m-Health technology to deliver secondary prevention programmes, nine studies utilized web-based technology, and seven studies utilized a combination of m-Health technology and web-based technology. Most of the studies utilized two or three components for their secondary prevention programme. Patient education was performed in twenty-one studies. m-Health technology were found to have a positive effect on medication adherence. Several studies including traditional cardiac rehabilitation programmes, showed improvement on heart-related risk factors.

The study found that evidence exists to support the use of e-Health secondary prevention programmes for patients with coronary artery disease, However, there is great variability in components and outcomes within the different modes of delivery. Therefore, larger studies are needed to determine the most efficient mode of delivery and components capable of addressing a favourable outcome for patients.
Read the article
The project has 4 PhD-candidates, 1 postdoctoral fellow and 3 master students. Several more master projects are being planned for. The main supervisor for all PhD projects is professor Tone Merete Norekvål.
Irene Valaker
The overall aim of the study was to develop knowledge of the multidimensional concept of continuity of care across care levels, with a focus on patients’ experiences, instrument adaptation and factors associated with health outcomes in patients after PCI.
Gunhild Brørs
The overall aim of the PhD project is to determine associations between health literacy, eHealth literacy and self-management, and to determine whether an expanded web-based cardiac rehabilitation program that is integrated into the primary health care services in a cost-efficient manner, can promote patient-reported self-management and health status.
Trond Pettersen
The overall aim of the PhD-project is to explore, describe and evaluate medication adherence, as well as determine consequences of non-adherence, before and after implementation of an eHealth intervention in patients after PCI.
Irene Instenes
The aim of the PhD-project is to examine particular conditions tied to patients in the age ≥ 80. Identifying phenotypes and determining risk factors for readmission and adverse events, in addition to addressing patients’ perspective on general health, individualized care- and rehabilitation will provide supporting evidence to enhance the care pathway.
Project leadership:
Principal investigator: Tone M. Norekvål, PhD, RN, Professor, University of Bergen and the Western Norway University of Applied Sciences. Chair of PROCARD research group, Department of Heart Disease, Haukeland University Hospital.
e-mail: tone.merete.norekval@helse-bergen.no
International coordinator and national coordinator Norway: Nina Fålun, MSc, Intensive Care Nurse, Clinical Nurse Researcher, Department of Heart Disease, Haukeland University Hospital, and Senior Lecturer at the Western Norway University of Applied Sciences.
Telephone: +4755974469
e-mail: nina.falun@helse-bergen.no
National coordinator Denmark: Tina Hansen, PhD, RN, Department of Cardiology, Zealand University hospital.
e-mail: tbh@regionsjaelland.dk